Who Will Read Our Scans?
Putting together results from our NIH-funded trial “Amelioration of Claustrophobia and Disruptive Motion in MR Imaging”, I became aware of an interesting phenomenon: The market may have become saturated with MRI scanners. The building of new state-of-the-art cancer hospitals or other specialty medical palaces, each with their own imaging facilities, in addition to free-standing and satellite MRI facilities may start doing to hospital systems what too many coffee shops did to Starbucks years ago. More capacity than the market can absorb and competition eat into profitability.
Before looking at the new data, I was under the assumption that the imaging business was still alive and well in spite of the rapid expansion of 3-D imaging such as CT and MRI that once threatened to bankrupt medical care. After alarm bells were raised in the last decade, efforts to cut down on overutilization, self-referral, and improper ordering of tests had some impact. Then the economic downturn, high patient co-pays, and drastic cuts in reimbursement finally ended the growth boom resulting in a decline of medical visits with imaging. Signs of saturation are being felt in urban centers (1).
When the Centers for Medicare and Medicaid Services (CMS) originally calculated technical cost reimbursement for use of these multimillion-dollar acquisitions they assumed that MRI scanners would be used 25% of a standard 50-hr working week and based reimbursement on a 25% utilization rate. Now the utilization rate is 90%. This means that a scanner has to run at full capacity 45 hours per week just to recoup the investment. To make more money facilities therefore start to press on personnel to work faster, get more patients done in less time, do faster room turn-over, extend shifts, and introduce night shifts for routine scanning. This will increase revenue until CMS and insurance companies take that into account further reducing reimbursement per case.
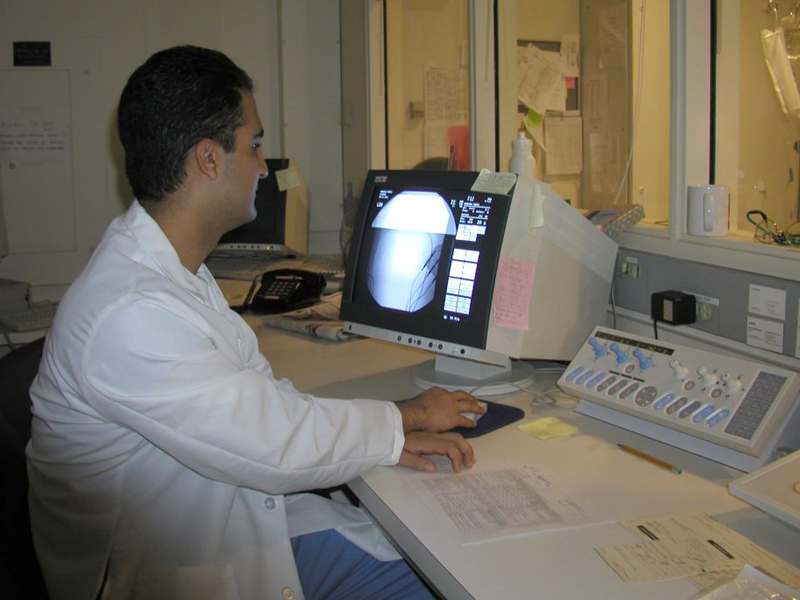
It is no wonder that MRI technologists are maximally stressed. On top of this, staff salaries are starting to be dependent on patient satisfaction. We have learned of managers who were fired for less than stellar ratings. Radiologists have to read one image every 3-4 seconds in an 8-hr workday to meet workload demand (2). Over lunch with a friend and colleague we were wondering the other day – who will read our scans when we need them? And also, if we ever end up in a hospital bed, will we agree with being brought to the MRI scanner at 2 o’clock in the morning for a routine follow-up because days are reserved for paying outpatients?
Originally I got into researching and developing nonpharmacologic adjuncts to help patients be more comfortable and have better outcomes during interventional radiological procedures. Comfort Talk® evolved and we started training teams in MRI to help claustrophobic patients and improve throughput (3). I have now come more and more to see the Comfort Talk® skills as a means for staff to remain sane in a system where patients are on the edge and the pressures on speed are immense. Fortunately meaningful staff-patient interactions using the Comfort Talk® techniques are actually faster as our research showed, and also much more pleasant for all participants (4). So I hope that if I ever need a scan, I have a Comfort Talk® trained technologist – then my films will be motionless, and the radiologist can have an easier time reading them.
References
- Duszak R. Medical imaging: Is the growth boom over? The Neiman Report, No.1, October 2012. Studies in Health Care and Economics. http://www.acr.org/~/media/ACR/Documents/PDF/Research/Brief 01/PolicyBriefHPI092012.pdf.
- McDonald RJ, Schwartz KM, Eckel LJ, Diehn FE, Hunt CH, Bartholmai BJ, et al. The effects of changes in utilization and technological advancements of cross-sectional imaging on radiologist workload. Acad Radiol. 2015 Sep;22(9):1191-8. http://www.ncbi.nlm.nih.gov/pubmed/26210525
- Norbash A, Yucel K, Yuh W, Doros G, Ajam A, Lang EV, et al. Effect of team training on improving MRI study completion rates and no show rates. Journal of magnetic resonance imaging : JMRI. 2016 http://www.ncbi.nlm.nih.gov/pubmed/27126735
- Lang EV, Benotsch EG, Fick LJ, Lutgendorf S, Berbaum ML, Berbaum KS, et al. Adjunctive non-pharmacological analgesia for invasive medical procedures: a randomised trial. Lancet. 2000 Apr 29;355(9214):1486-90. http://www.ncbi.nlm.nih.gov/pubmed/10801169
