Radiology – The Specialty With an Inferiority Complex?
Radiology – the specialty that has a hard time to promote itself. Could it suffer from an inferiority complex? Or from being out of (patient) touch?
What gave me the incentive to write today was an article by Drs. Gunderman and Fogler in Academic Radiology about “Educating Radiologists about Pain in Radiology.” The authors amassed 37 references dating back to the 17th century philosopher Descartes and listing all kind of pain reports in all kind of specialties– except some fundamental work that has been done about acute pain in the radiology setting and how to ameliorate it (just a few samples 1-7). I responded by a Letter to the Editor which just got published to set the record straight.
After all, the controlled environment of the radiology department allowed to evaluate what happens during potentially painful interventions. It showed how anxiety and pain potentiate each other, and under standard care conditions increase linearly over time. And that increase is relatively independent of the invasiveness of the procedure and the amount of drugs given! Fortunately a short Comfort Talk intervention can profoundly change this mechanism of pain processing and allow patients to bolster their own coping resources.
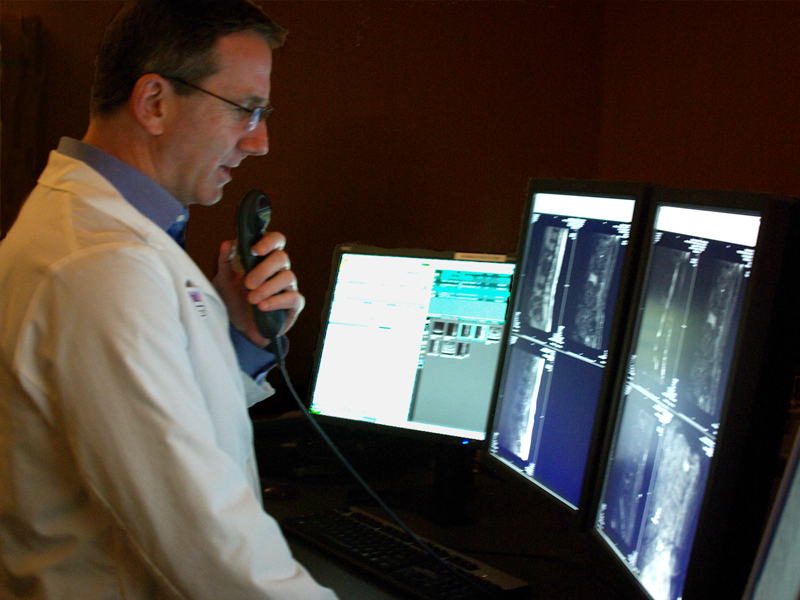
I was puzzled that the authors didn’t think to look into the radiology literature on the topic. Could there have been an assumption that radiologists don’t investigate patient issues? The old joke goes that if you want to hide a 100-dollar bill from a radiologist you pin it on the patient. The relative lack of giving credit to the specialty is not new. While diagnostic and interventional radiology have greatly contributed to the progress of medical diagnosis and minimally invasive surgical treatments, the specialty usually makes little fanfare about its successes. Possibly sitting in a dark room and reading films all day may be attractive to a certain breed of individuals. Then there are also those who swing catheters and push the envelope creatively towards new treatments. Perhaps the specialty should have better headed the advice by Dr. Charles Dotter who invented angioplasty. He warned that if his “ fellow angiographers prove unwilling or unable to accept or secure for their patients the clinical responsibilities attendant on transluminal angioplasty, they will become high-priced plumbers facing forfeiture of territorial rights based solely on imaging equipment others can obtain and skill still others can learn.”
Even after interventionalists are now busily taking care of their patients in clinics and hospital admission for years, there are large swath of the population who never heard about an interventional radiologists. I guess we are just not tooting our horn enough.
References
- Lang EV, Benotsch EG, Fick LJ, et al. Adjunctive non-pharmacological analgesia for invasive medical procedures: a randomised trial. Lancet 2000;355:1486-1490.
- Lang EV, Berbaum KS, Faintuch S, et al. Adjunctive self-hypnotic relaxation for outpatient medical procedures: a prospective randomized trial with women undergoing large core breast biopsy. Pain 2006;126:155-164.
- Lang EV, Berbaum KS, Pauker SG, et al. Beneficial effects of hypnosis and adverse effects of empathic attention during percutaneous tumor treatment: when being nice does not suffice. J Vasc Interv Radiol 2008;19:897-905.
- Flory N, Lang EV. Distress in the radiology waiting room. Radiology 2011;260:166-173.
- Lang EV, Berbaum KS, Lutgendorf SK. Large-core breast biopsy: abnormal salivary cortisol profiles associated with uncertainty of diagnosis. Radiology 2009;250:631-637.
- Lang EV, Tan G, Amihai I, Jensen MP. Analyzing acute procedural pain in clinical trials. Pain 2014;155:1365-1373.
- In Ray C (ed) Pain management in Interventional Radiology. Cambridge University Press, Cambridge, New York, Melbourne, 2008
